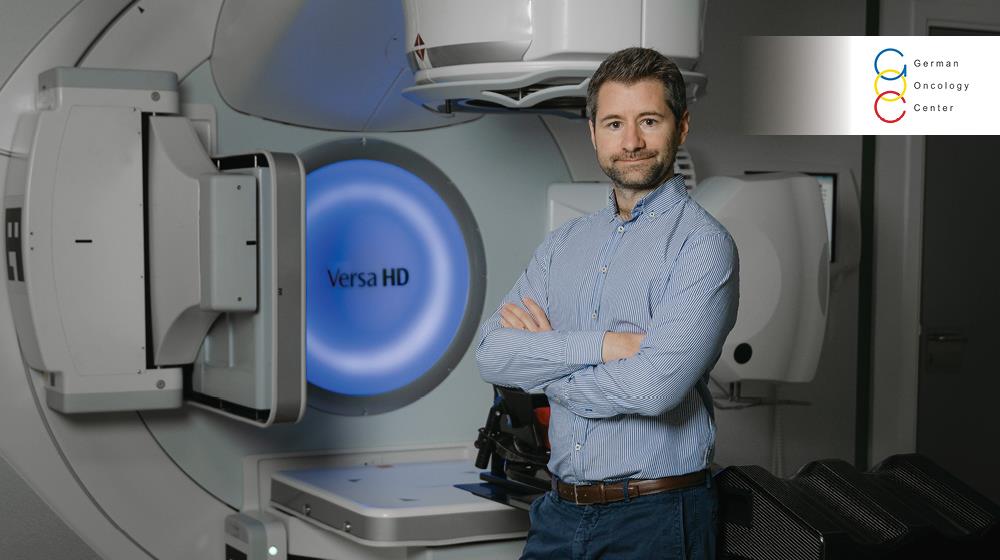
"At this stage, AI in healthcare should be seen as an assistant, not a decision-maker. Algorithms can handle well-defined, repetitive tasks – like identifying anatomical structures or flagging abnormal scan findings – but healthcare decisions are often complex and context-dependent, which is information the AI doesn’t usually have access to," Paul Doolan, General Coordinator of Medical Physics, Director of AI at the German Oncology Center proposes.
In a recent interview with GOLD magazine, he goes on to elaborate, "As such, human judgment remains essential. We don’t expect AI to replace our doctors, but rather to augment their capabilities."
The expert also talks about the specific AI tools the Limassol-based German Oncology Center has adopted and their benefits.
In addition, he, among other things, discusses the biggest bottlenecks in integrating AI solutions, shares which AI trend or technology he is keeping a particularly close eye on, and reveals the one AI breakthrough he believes will be a game-changer in the medical industry.
What are the specific AI tools that you have adopted? How well did they integrate with your existing infrastructure? Did they require specific customisation to work effectively?
One key treatment in oncology is radiotherapy, where high-energy X-rays are delivered to target and destroy cancer cells. This requires precise planning, using CT scans to map the tumour and surrounding organs. Traditionally, this ‘contouring’ process – manually drawing organs like the heart, lungs or kidneys – could take up to 1.5 hours for complex cases. With recent advances in deep learning, we can now generate these contours in under a minute. Clinicians still verify and make minor adjustments but the process now takes only 2–5 minutes, depending on the site.
Since 2019, we’ve tested seven commercial auto-contouring tools and contributed to national UK guidelines. The solution we chose integrates seamlessly into our workflow with no disruption. It’s customisable to different anatomical sites but intentionally not self-learning, which is vital in healthcare. We need consistency, not unpredictable updates.
Have these AI deployments led to revenue growth, cost savings, or improved customer retention? Can you quantify these improvements? And how long will it take before you see a measurable return on your investment?
The tool offers four major benefits: consistency, accuracy, new insights and time savings. Consistency is crucial – AI always produces the same result for a given scan, unlike manual methods which vary between clinicians or even for the same clinician on different days. This reliability helps when evaluating treatment efficacy and side effects across patient groups. Accuracy is higher: many blinded studies show that clinicians often prefer AI-generated contours to human-drawn ones. At our institute, some now consider the AI output the new standard.
AI also allows us to analyse more anatomical structures, potentially uncovering new correlations between radiation exposure and side effects. But the biggest benefit is time saving. Reclaiming 19–92 minutes per case allows clinicians to focus on patient care, precision targeting and staying updated on innovation, all of which are far more valuable uses of their time.
What have been the biggest bottlenecks in integrating AI solutions? How did you overcome these challenges?
The main challenge isn’t technical – it’s training staff and evolving workflows. Our team is highly skilled but AI demands a shift in mindset and responsibilities. Thankfully, our staff have shown great willingness to adapt. What helped most to get our staff on board with the change was showing the tool’s impact on our own clinical data. It’s one thing to see a demo at a conference; it’s another to see it work effectively in your own hospital.
As AI continues to transform the workplace, how has the German Oncology Center adapted? How have employees responded and what steps have you taken to support this transition?
Our hospital sees the clear potential of AI to improve workflows, imaging speed and reduce patient exposure. Auto-contouring in radiotherapy has been evaluated since 2019; AI-enhanced MRI and nuclear medicine followed in 2023 and 2024. This expansion has required staff to learn new skills, such as evaluating, commissioning and deploying AI tools. As adoption increases, so does the need for coordinated deployment, auditing and governance. In January 2025, we established an AI department to act as the hospital’s gatekeeper for all future deployments. I now lead this team, with a clear vision: to establish ourselves as leaders in safe, effective AI deployment, both within Cyprus and across Europe.
In your industry, what types of decisions can realistically be entrusted to an algorithm? And do you think that AI will ever be capable of handling the novelty and ambiguity of executive-level decision-making?
At this stage, AI in healthcare should be seen as an assistant, not a decision-maker. Algorithms can handle well-defined, repetitive tasks – like identifying anatomical structures or flagging abnormal scan findings – but healthcare decisions are often complex and context-dependent, which is information the AI doesn’t usually have access to. As such, human judgment remains essential. We don’t expect AI to replace our doctors, but rather to augment their capabilities.
Over time, I can see a future where AI takes on more decision-support roles, such as providing second opinions, highlighting patterns across large datasets or suggesting treatment paths based on similar cases. What I can envision, however, is using multiple AI tools to analyse the same image set and if at least three independently trained systems produce the same result – especially for normal cases – we could consider auto-reporting. Since these tools are built differently and trained on separate datasets, their agreement adds confidence. It wouldn’t replace clinical oversight but could help reduce the workload burden.
Which AI trend or technology are you watching closely and which do you think are more marketing fluff than substance?
We are currently investigating options for AI in computer-assisted diagnosis of radiology examinations such as CT, mammography and MRI. Radiology demand is growing but radiologist numbers are not. If AI can accurately highlight areas of concern, it could significantly reduce reading time and lighten workloads.
On the more speculative side, ‘agentic AI’ is generating a buzz – systems that can autonomously collect and synthesise patient information from various platforms. In theory, this could streamline one of the most inefficient parts of a doctor’s job, which involves collecting the patient history. I’d love to see it happen but, so far, it’s more concept than clinic-ready.
What is the one AI breakthrough that you believe will be a game-changer for your industry?
AI scribes could revolutionise clinical consultations. Today, doctors often sit behind a screen, typing notes in real-time – a practice that can feel impersonal to patients. With AI scribes, the conversation is transcribed and summarised automatically, with key information uploaded to the electronic health record. The doctor only needs to review and confirm the notes. This reduces admin burden and improves patient experience. More time is spent listening and less time typing. It humanises the consultation while increasing efficiency, a true win-win.
This interview first appeared in the April edition of GOLD magazine. Click here to view it.